Signs of gastric constipation in cats. Stomach diseases in cats: diseases of the gastrointestinal tract, symptoms and treatment
1. Oral cavity (Cavum oris)
Food, entering the initial section of the digestive apparatus through the oral opening, enters the oral cavity, the skeleton of which is the upper and lower jaws, palatine and incisive bones. The hyoid bone, located inside the oral cavity, serves as a place of fixation for the muscles of the tongue, pharynx and larynx. The oral cavity extends orally from the lips, and aborally ends with the pharynx and passes into the pharynx. The dental edge of the closed jaws and lips form the vestibule of the oral cavity. Behind the vestibule is the oral cavity itself. The vestibule communicates with external environment oral slit. The oral fissure begins at the junction of the upper and lower lips, called the angle of the mouth.
Appearance of the oral cavity
Lips- upper and lower muscle-skin folds, covered on the outside with hair and on the inside with mucous membrane. Outside, the upper lip is sagittally divided by a deep groove - a filter, passing towards the nasal septum. On the upper lip there are hard whiskers, collected in 2 side tufts - mustaches.
Cheeks are a continuation of the lips behind their commissure and form the lateral walls of the oral cavity. The cheeks of cats are relatively small, thin, and covered with hair on the outside. Their inner surface is smooth, and the ducts of the salivary glands open on it.
Teeth- durable organs of the oral cavity that serve to capture and hold food, bite it, crush and grind it, as well as defend and attack.


Adult cats have 30 teeth, 16 of which are in the upper jaw and 14 in the lower jaw. Cats are carnivores by nature, which largely reflects the arrangement of their teeth. Cats have six front teeth and two canines in each jaw. These teeth are involved in the process of biting into meat and then tearing it. Cats have only 6 premolars and 2 molars in the upper jaw and 4 premolars and 2 molars in the lower jaw. Cats are also characterized by an increased size of the upper 4th molar (also called the “carnivore tooth”) and the 1st lower incisor. Due to the arrangement of these “carnivorous teeth”, eating food occurs according to the “scissor principle”, which is extremely effective when cutting raw meat.
STRUCTURE OF TEETH
A tooth consists of dentin, enamels And cement.
Schematic representation of the cutter:

Dentine- tissue that forms the basis of the tooth. Dentin consists of a calcified matrix penetrated by dentinal tubules containing processes of odontoblast cells lining the tooth cavity. The intercellular substance contains organic (collagen fibers) and mineral components (hydroxyapatite crystals). Dentin has different zones that differ in microstructure and color.
Enamel- a substance covering dentin in the crown area. It consists of crystals of mineral salts, oriented in a special way to form enamel prisms. Enamel does not contain cellular elements and is not tissue. The normal color of enamel is from white to cream with a yellowish tint (distinguishable from plaque).
Cement- tissue covering dentin in the root area. The structure of cement is close to bone tissue. Consists of cementocyte and cementoblast cells and a calcified matrix. Nutrition of cement occurs diffusely from the periodontium.
Inside there is tooth cavity, which is divided into coronalcavity And root canal, opening with the above hole in the apex of the tooth. Fills the dental cavity dental pulp, consisting of nerves and blood vessels immersed in loose connective tissue and providing metabolism in the tooth. Distinguish coronal And root pulp.
Gum- mucous membrane that covers the dental edges of the corresponding bones, tightly fused with their periosteum.
The gum covers the tooth in the neck area. It is abundantly supplied with blood (tendency to bleeding), but relatively poorly innervated. The grooved depression located between the tooth and the free edge of the gum is called the gingival sulcus.
The periodontium, alveolar wall and gums form supporting apparatus of the tooth - periodontium.
Periodontium- provides attachment of the tooth to the dental alveolus. It consists of the periodontium, the wall of the dental alveoli and the gums. The periodontium performs the following functions: supporting and shock-absorbing, barrier, trophic and reflex.
The teeth are distributed as follows: 12 incisors (I), 4 canines (C), 10 premolars (P) and 4 molars (M). Thus, the dental formula is as follows:
![]()
All teeth are of pronounced short-crown type.
There are 4 types of teeth: incisors, fangs And permanent teeth: preradical(false, small molars), or premolars And truly indigenous, or molars that do not have milk precursors.
Teeth arranged in order in a row form top
and lower dental arches (arcades)
.
Incisors- small, with uneven edges and 3 protruding points. Each root is single. The lateral incisors are larger than the medial ones, and the incisors of the upper jaw are larger than those of the lower jaw.
Schematic representation of the incisors:

Behind the incisors are located fangs. These are long, strong, deep-set teeth with a simple root and a rounded crown. When the jaws are closed, the lower canines lie laterocaudal to the upper ones. Behind the fangs on each jaw there is an edge free from teeth.
Schematic representation of fangs:

Molars of the upper dental arch.
Premolars are located behind the diastema; there are 3 pairs of them on the upper jaw
and 2 pairs on the bottom. The first premolar of the upper jaw is small,
with a simple crown and a simple root. The second premolar is larger, it has 4 projections - a large central one, a small cranial one
and 2 small caudal ones. The most massive tooth is the third premolar: it has 3 large protrusions located along the length
and small projections lying on the medial side of the first; the root of the tooth has 3 processes.
Schematic representation of premolars:

Upper dental arcade of a seven-month-old cat:

Molars located caudal to the last premolar in the upper jaw. These are small teeth with 2 projections and 2 roots.
Schematic arrangement of molars:

Molars of the lower dental arch.
In the lower arcade 2 premolar; they are identical in size and shape. The crown of each premolar bears 4 projections - one large, one small in front and two more behind. Each premolar has
2 roots.
Molar the lower jaw is the most massive in the arcade and has
2 protrusions and 2 roots. The molars sit obliquely in the sockets, so that when the jaws are closed, the teeth of the upper jaw adjoin the lower teeth from the inside.
The lower dental arcade of a seven-month-old cat:

Baby teeth appear in kittens soon after birth.
They are smaller in size than the permanent ones and less developed. Their color
milky white. There are fewer primary teeth than permanent teeth because molars have no predecessors.
The dental formula of primary teeth is as follows: ![]()
MECHANICAL DIGESTION
Digestion in the oral cavity occurs mainly mechanically; when chewing, large fragments of food are broken into pieces and mixed with saliva.
Mechanical digestion also increases the area exposed to digestive enzymes. The position of teeth is closely related to the natural diet various types animals and indicates their natural eating behavior and their preferred diet.
ORAL CAVITY
The oral cavity itself is separated from above, from the side of the nasal cavity, by the hard palate, from the pharynx by the soft palate, and is limited in front and on the sides by dental arcades.
Solid sky arched like a vault. Its mucous membrane forms 7 - 8 caudally concave transverse ridges - palatine ridges, between which the papillae are located. In the anterior part behind the incisors there is a small incisive papilla;
to the right and left of it lie the slit-like nasopalatine canals, which are the excretory ducts of the nasopharynx organ.
In the aboral direction, in the area of the choanae, the hard palate passes into the soft palate without a visible boundary.
Soft palate or velum- is a continuation of the hard palate and is a fold of the mucous membrane that covers the entrance to the choanae and pharynx. The soft palate is based on special muscles: the levator velum palatine, the tensor velum palatine, and the palatine muscle that shortens it after the act of swallowing. The velum palatine hangs from the end of the bony palate and, in a calm state, its free edge touches the root of the tongue, covering the pharynx, the exit from the oral cavity into the pharynx.
The free edge of the velum is called the arch of the palate. The palatine arch, together with the pharynx, forms the velopharyngeal arches, and with the root of the tongue - the palatoglossus arches. Aborally on the sides of the root of the tongue, in the tonsil sinuses there is one palatine tonsil.
SALIVARY GLANDS
Cats have 5 pairs of salivary glands: parotid, submandibular, sublingual, molar and infraorbital.
Layout of the salivary glands of a cat:

1 - parotid
2 - submandibular
3 - sublingual
4 - radical
5 – infraorbital
Parotid salivary gland located ventral to the external auditory canal under the cutaneous muscles. It is flat, has a lobular structure, and borders orally with the large masseter muscle. The excretory ducts of the individual lobules of the gland merge to form the common parotid (stenon) duct. It passes cranially as part of the fascia covering the large masticatory muscle, at the cranial edge of the muscle it turns inward, goes under the mucous membrane and opens into the buccal vestibule of the mouth opposite the last premolar with the salivary papilla. Along the duct there are one or more small accessory parotid salivary glands.
Submandibular gland rounded, lies ventral to the previous one near the large masseter muscle and consists of individual glandular lobules connected by connective tissue. The excretory duct of the submandibular gland is located on its inner surface, it stretches forward under the base of the tongue and opens at the bottom of the oral cavity with a sublingual wart, next to which the duct of the sublingual gland opens.
Sublingual gland elongated, conical, its base is adjacent to the submandibular gland, stretching 1-1.5 cm along its duct. The excretory duct of the sublingual gland is located on the ventral side; in its course it accompanies the duct of the submandibular gland, following first dorsally and then ventrally from it.
Indigenous salivary gland, absent in other domestic animals, in the cat it is located at the cranial edge of the large masseter muscle, between the mucous membrane of the lower lip and the orbicularis oris muscle. It is a flat formation that widens caudally and tapers orally. The anterior edge of the gland is visualized at the level of the canine. It has several ducts that open directly into the oral mucosa.
Orbital or zygomatic gland Of all domestic animals, only dogs and cats have it. It has a round shape and reaches a length of 1.5 cm. It is located medial to the zygomatic arch in the lower part of the orbit. The ventral edge is located behind the molar. Its large excretory duct and additional small ducts open into the oral cavity 3 - 4 mm caudal to the upper molar.
ENZYMATIVE DIGESTION
Saliva is secreted into the oral cavity by five pairs of salivary glands. Typically, a small amount of saliva is present in the mouth, but its flow may increase if the animal sees or smells food.
Salivation continues as food enters the oral cavity, and its effect is enhanced by the chewing process.
Saliva is 99% water, while the remaining 1% is mucus, inorganic salts and enzymes. Mucus acts as an effective lubricant and promotes swallowing, especially dry food. Unlike humans, cats lack the starch-digesting enzyme amylase in their saliva, which prevents the rapid absorption of starch in the mouth. The absence of this enzyme is consistent with the observed carnivorous behavior of cats that tend to consume foods low in starch.
Language- a muscular, movable organ lying at the bottom of the oral cavity.
Tongue and dorsally open pharynx:

Language in cats it is elongated, flat, widened in the middle and slightly narrowed at the end. When the oral cavity is closed, the tongue completely fills it. In terms of external shape, the tongue of cats is long, wide and thin.
The root of the tongue extends from the molars to the epiglottis and is closely connected to the hyoid bone.
The body of the tongue is almost twice as long as the root; it is located between the molars and has a dorsal back and 2 lateral surfaces. At the border with the apex below, the body forms a median fold containing parts of both geniohyoid muscles, this is the frenulum of the tongue. Folds are directed from the caudal end of the body to the epiglottis. The tip of the tongue rests with its free end against the incisor teeth.
On the back of the tongue and in the region of its apex, the mucous membrane is dotted with many rough, keratinized filiform papillae; their apices are directed caudally. Fungiform papillae are located on the surface of the dorsum, the largest of them lie along the edges of the tongue. Large ridge-shaped, or grooved, papillae in two caudally converging rows of 2-3 in each are located at the root of the tongue. The ventral surface and lateral edges of the tongue are smooth, soft, and free of papillae.
The muscles of the tongue consist of longitudinal, transverse and perpendicular bundles. The first ones go from the root of the tongue to its apex, the second ones - from the middle connective tissue septum of the tongue to the sides, the third ones run vertically from the back of the tongue to the bottom surface. These are the actual muscles of the tongue, located in its thickness;
with their help, the tongue can be shortened, thickened and flattened. In addition, there are muscles that connect the tongue to the bones of the oral cavity.
Genioglossus muscle passes from the symphysis of the mandible, where it originates on the medial surface; its fibers pass dorsally, located above the geniohyoid muscle, diverge; of these, the cranial ones reach the tip of the tongue, the caudal ones end at the root of the tongue. Dorsally, the muscle is mixed with the muscle of the same name on the opposite side.
Function: pulls the root of the tongue forward and the top of it to the side.
Lingual lateral muscle arises from the mastoid process of the temporal bone, from the ligament connecting the edge of the external auditory canal and the angular process of the mandible, and from the proximal part of the cranial horns of the hyoid bone. It passes into the lateral part of the tongue between the digastric and lingual main muscles, then, diverging, goes forward to the tip of the tongue, where it ends.
Function: pulls the tongue back with bilateral action, shortening it when swallowing; with unilateral action, turns the tongue to the side.
2. Pharynx (Pharynx)
Pharynx a mobile muscular-cavitary organ in which the digestive tract crosses, going through the pharynx from the oral cavity to the pharynx and further to the esophagus and the respiratory tract - through the choanae to the pharynx and further to the larynx.
Appearance of the pharynx:

Due to the fact that the cross-section of the digestive and respiratory tracts occurs in the pharynx, its mucous membrane, with the help of folds - the velopharyngeal arches, is divided into the upper, respiratory, and lower, digestive parts. The respiratory part is a continuation of the choanae, and is therefore called the nasal part of the pharynx, or nasopharynx. Near the choanae, a paired opening of the auditory tubes opens into the lateral wall of the pharynx. The digestive, or laryngeal, part in front borders the pharynx, being separated from it by the velum palatine, and is a caudal continuation of the oral cavity, rests against the epiglottis at the back and then, located on top of the larynx, follows towards the esophagus, which lies in this area above the trachea.
The muscles of the pharynx are striated, represented constrictors And dilators.
Cranial constrictor The pharynx consists of 2 paired muscles - the pterygopharyngeal and glossopharyngeal.
Pterygopharyngealmuscle flat, triangular, begins at the apex of the uncinate process of the pterygoid bone. Heading caudally, the muscle diverges under the medial constrictor. Some of the fibers are attached to the median suture of the pharynx, the dorsal fibers are attached to the base of the pterygoid bone, the ventral ones run along the length of the pharynx and end on the larynx.
Glossopharyngeal muscle begins on the geniohyoid muscle, passes as a thin ribbon outside the cranial horns of the hyoid bone, turns dorsally and attaches to the middorsal suture of the pharynx.
Middle, or sublingual, constrictor pharynx - a thin muscle covering the middle part of the lateral surface of the pharynx. It begins with two heads - on the cranial horns and the free caudal horn of the hyoid bone; attaches to the dorsal suture of the pharynx and the base of the sphenoid bone.
Caudal or laryngeal constrictor The pharynx begins on the lateral side of the thyroid and cricoid cartilages. The fibers run dorsally and cranially and attach to the pharyngeal suture.
Stylopharyngeal muscle begins at the apex of the mastoid process of the temporal bone. The ribbon-shaped abdomen extends ventrocaudally and is attached to the dorsal wall of the pharynx and larynx. Laterally, the muscle is covered by the middle and caudal constrictors. Contraction of the pharyngeal muscles underlies the complex act of swallowing, which also involves the soft palate, tongue, esophagus and larynx. At the same time, the pharyngeal levators pull it upward, and the compressors successively backwards narrow its cavity, pushing the food bolus into the esophagus. At the same time, the larynx rises and tightly covers the epiglottis, due to pressure on it with the root of the tongue. In this case, the muscles of the soft palate pull it upward and caudally so that the velum palatine rests on the palatopharyngeal arches, separating the nasopharynx. During breathing, the shortened velum palatine hangs obliquely downward, covering the pharynx, while the epiglottis, built of elastic cartilage and directed upward and forward, provides access to a stream of air into the larynx.
3. Esophagus (Oesophagus)
Esophagus It is a cylindrical tube following the pharynx, flattened at the top and bottom.
Esophageal endoscopy:


It is the initial section of the foregut and in structure is a typical tube-shaped organ. The esophagus is a direct continuation of the laryngeal part of the pharynx.
Usually the esophagus is in a collapsed state. The mucous membrane of the esophagus along its entire length is collected in longitudinal folds that straighten out as the food coma passes.
The submucosal layer contains many mucous glands that improve the sliding of food. The muscular layer of the esophagus is a complex multi-level striated layer. The outer membrane of the cervical and thoracic parts of the esophagus is connective tissue adventitia, and the abdominal part is covered with visceral peritoneum. The attachment points of the muscle layers are: laterally - the arytenoid cartilages of the larynx, ventrally - the annular cartilage, and dorsally - the tendon suture of the larynx.
The diameter of the esophagus is relatively constant throughout its entire length and reaches 1 cm during the passage of the food bolus. The esophagus is divided into cervical, thoracic and abdominal sections. Upon exiting the pharynx, the esophagus is located dorsal to the larynx and trachea, covering the bodies of the cervical vertebrae from below, then descends to the left side of the trachea and in the area of its bifurcation returns again to the midline. In the chest cavity, it lies in the mediastinum, passing over the base of the heart and under the aorta. It enters the abdominal cavity through the esophageal opening of the diaphragm, which lies approximately 2 cm ventral to the vertebral column. The abdominal region is very short.

1 - language
2 - pharynx and larynx
3 - esophagus in a collapsed state
4 – stomach
During the process of swallowing, a lump of unchewed food formed by the tongue enters the esophagus. The esophagus does not secrete digestive enzymes, but the cells of the esophagus secrete mucus, which serves to lubricate peristalsis, the automatic wave-like muscle contractions that are stimulated by the presence of food in the esophagus and allow it to move through the gastrointestinal tract. The process of moving food from the mouth to the stomach takes only a few seconds.
4. Stomach (Ventriculus)
Stomach is the organ of the digestive tract where food is retained and exposed chemical treatment. The cat's stomach is single-chamber, intestinal type. It is an extension of the digestive tube behind the diaphragm.

1 - pyloric part of the stomach
2 - cardiac part of the stomach
3 - fundic part of the stomach
4 - exit of the duodenum
5 - cardial opening (entrance of the esophagus)
Appearance of the opened stomach:

TOPOGRAPHY OF THE CAT'S STOMACH
The stomach is located in the anterior part of the abdominal cavity to the left of the midline, in the plane of the IX-XI intercostal space and in the region of the xiphoid process. The anterior, or diaphragmatic, wall is adjacent to the diaphragm only dorsally; the cardiac part of the stomach does not touch the diaphragm, so a small segment of the esophagus passes into the abdominal cavity. The posterior, visceral wall is adjacent to the intestinal loops.
Contrast radiograph of a cat's stomach:

STRUCTURE OF A CAT'S STOMACH
Scheme cross section stomach, indicating the anatomical and functional elements:

In the enlarged initial part of the stomach, which lies on the left, there is the inlet of the esophagus. In the narrowed-elongated part lying to the right and below there is a second opening leading to the duodenum, the pyloric opening, and the pylorus.
In accordance with this, the cardiac and pyloric parts of the stomach are distinguished. The concave and convex sections located between them are called the lesser and greater curvature. The concave lesser curvature faces cranially and to the right. The convex greater curvature is directed caudally and to the left. The middle part of the stomach on the side of the greater curvature is called the fundus of the stomach.


In an empty stomach mucous membrane collected in longitudinal folds running parallel to each other. The surface of the gastric mucosa is about 1/5 - 1/6 of the total surface of the intestinal mucosa.
Muscularis The stomach is well developed and is represented by three layers.
Ultrasound image of the wall of a healthy stomach:

The superficial thin longitudinal layer is directed from the esophagus to the pylorus. In the area where the bottom and pyloric glands are located, the circular, or circular, layer of fibers reaches its greatest expression. In the left part of the stomach, the internal oblique layer predominates. As they approach the pylorus, the muscle walls thicken and, at the border with the duodenum, break off in the form of a thickened annular ridge. This strong muscular sphincter is called the sphincter muscle, or constrictor pylorus. In the constrictor area, the mucous membrane is also collected in longitudinal folds.
The outside of the stomach is covered serosa, which at the lesser curvature passes into the lesser omentum, in the area of greater curvature into the greater omentum. The first connects the stomach to the liver through the hepatogastric ligament. This ligament on the left merges with the ligament of the liver and esophagus and on the right - with the ligament of the liver and duodenum. The greater omentum, from the stomach to the lower back, forms the omental sac.
On the right, near the kidney, at the caudal vena cava and portal vein, there is an entrance to the omental sac. The spleen, located between the layers of the greater omentum, connects to the stomach through the gastrosplenic ligament.
In progress embryonic development the stomach, as part of a straight digestive tube, undergoes two 180° rotations. One in the frontal plane counterclockwise and the other in the segmental plane.
FUNCTIONS OF THE STOMACH
The stomach has several functions: it serves to temporarily store food and controls the rate at which food enters the small intestine.
The stomach also secretes enzymes necessary for the digestion of macromolecules.
The stomach muscles regulate motility, allowing food to move aborally (away from the mouth), and aid digestion by mixing and grinding food.
PHASES OF STOMACH SECRETION
Gastric secretion is regulated by complex processes of nervous and hormonal interaction, due to which secretion is produced at the right time and in the required volume. The secretion process is divided into three phases: cerebral, gastric and intestinal.
Brain phase
The medullary phase of secretion is initiated by the anticipation of food intake and the sight, smell and taste of food, which stimulates the secretion of pepsinogen, although gastrin and hydrochloric acid are also released in small quantities.
Gastric phase
The gastric phase is initiated by mechanical stretching of the gastric mucosa, a decrease in acidity, as well as products of protein digestion. In the gastric phase, the main secretion product is gastrin, which also stimulates the secretion of hydrochloric acid, pepsinogen and mucus. Gastrin secretion slows down sharply if the pH drops below 3.0 and may also be controlled by peptic hormones such as secretin.
or enteroglucagon.
Intestinal phase
The intestinal phase is initiated by both mechanical distension of the intestinal tract and chemical stimulation with amino acids and peptides.
5. Small intestine (Intestinum tenue)
Small intestine is a narrowed section of the intestinal tube and consists of many loops that occupy most of the space of the abdominal cavity. The total length of the intestine is almost 4 times the length of the body and is about 1.98 m, with the small intestine accounting for 1.68 m and the large intestine 0.30 m. The mucous membrane of the small intestine is velvety due to the presence of villi. The muscular coat is represented by a longitudinal and circular layer of smooth muscle fibers. The serous membrane passes to the intestine from the mesentery.
According to its position, the small intestine is divided into duodenum, jejunum and ileum. Their length is, respectively, 0.16; 1.45; 0.07 m.

Ultrasound of the small intestine:

The wall of the thin section is richly vascularized. Arterial blood flows through the branches of the cranial mesenteric artery, and to the duodenum also through the hepatic artery. Venous drainage occurs in the cranial mesenteric vein, which is one of the roots of the portal vein of the liver.
Lymphotok from the intestinal wall comes from the lymphatic sinuses of the villi and intraorgan vessels through the mesenteric (intestinal) lymph nodes into the intestinal trunk, which flows into the lumbar cistern, then into the thoracic lymphatic duct and the cranial vena cava.
Nervous support The thin section is represented by branches of the vagus nerve and postganglionic fibers of the solar plexus from the semilunar ganglion, which form two plexuses in the intestinal wall: intermuscular (Auerbach) between the layers of the muscular layer and submucosal (Meissner) in the submucosal layer.
Control of intestinal activity by the nervous system is carried out both through local reflexes and through vagal reflexes involving the submucosal nerve plexus and intermuscular nerve plexus.
Bowel function is regulated by the parasympathetic nervous system. Control is directed from the medullary portion of the vagus nerve to the small intestine. The sympathetic nervous system (control directed from the ganglia in the paravertebral sympathetic trunk) plays a less important role. The processes of local control and coordination of motility and secretion of the intestine and associated glands are of a more complex nature; nerves, paracrine and endocrine chemicals take part in them.
TOPOGRAPHY
The thin section begins from the pylorus of the stomach at the level of the 12th rib, is covered ventrally by the leaves of the greater omentum, and is limited dorsolaterally by the thick section. There are no clear boundaries between the sections of the small intestine, and the identification of individual sections is mainly topographical in nature. Only the duodenum is most clearly distinguished, which is distinguished by its large diameter and topographic proximity to the pancreas.
MININGS OF THE INTESTINAL
The functional features of the small intestine leave an imprint on its anatomical structure.
There are mucous membrane and submucosal layer, muscular (external longitudinal and internal transverse muscles) and serous membranes of the intestine.

Mucous membrane forms numerous devices that significantly increase the suction surface.
These devices include circular folds, or Kirkring folds, in the formation of which not only the mucous membrane is involved, but also the submucosal layer and villi, which give the mucous membrane a velvety appearance.
The folds cover 1/3 or 1/2 of the circumference of the intestine. The villi are covered with a special bordered epithelium, which carries out parietal digestion and absorption. The villi, contracting and relaxing, perform rhythmic movements with a frequency of 6 times per minute, due to which they act as a kind of pumps during suction.
In the center of the villus there is a lymphatic sinus, which receives fat processing products.
Each villus from the submucosal plexus contains 1-2 arterioles, which break up into capillaries. Arterioles anastomose with each other and during absorption all capillaries function, while during a pause there are short anastomoses. Villi are thread-like outgrowths of the mucous membrane, formed by loose connective tissue rich in smooth myocytes, reticulin fibers and immunocompetent cellular elements, and covered with epithelium. The length of the villi is 0.95-1.0 mm, their length and density decreases in the caudal direction, that is, in the ileum the size and number of villi are much smaller than in the duodenum and jejunum.
The mucous membrane of the thin section and villi is covered with a single-layer columnar epithelium, which contains three types of cells: columnar epithelial cells with a striated border, goblet exocrinocytes (secrete mucus) and gastrointestinal endocrinocytes.
Mucous membrane of the thin section is replete with numerous parietal glands - common intestinal, or Lieberkühn glands (Lieberkühn's crypts), which open into the lumen between the villi. The number of glands averages about 150 million (in the duodenum and jejunum there are 10 thousand glands per 1 cm 2 of surface, and 8 thousand in the ileum). The crypts are lined with five types of cells: epithelial cells with a striated border, goblet glandulocytes, gastrointestinal endocrinocytes, small borderless cells of the crypt bottom (stem cells of the intestinal epithelium) and enterocytes with acidophilic granules (Paneth cells). The latter secrete an enzyme involved in the breakdown of peptides and lysozyme.
The duodenum is characterized by tubular-alveolar duodenal, or Bruner's glands, which open into crypts. These glands are a continuation of the pyloric glands of the stomach and are located only on the first 1.5-2 cm of the duodenum.
The final segment of the thin section (ileum) is rich in lymphoid elements, which lie in the mucous membrane at different depths on the side opposite to the attachment of the mesentery, and are represented by both single (solitary) follicles and their clusters in the form Peyer'splaques. Plaques begin in the final part of the duodenum.
The total number of plaques is from 11 to 25, they are round or oval in shape, length from 7 to 85 mm, and width from 4 to 15 mm. The lymphoid apparatus takes part in the digestive processes. As a result of the constant emigration of lymphocytes into the intestinal lumen and their destruction, interleukins are released, which have a selective effect on the intestinal microflora, regulating its composition and distribution between the thin and thick sections. In young organisms, the lymphoid apparatus is well developed, and the plaques are large. With age, a gradual reduction of lymphoid elements occurs, which is expressed in a decrease in the number and size of lymphatic structures.
Muscularis represented by two layers of smooth muscle tissue: longitudinal And circular, and the circular layer is better developed than the longitudinal one. The muscular layer provides peristaltic movements, pendulum-like movements
and rhythmic segmentation, which moves and mixes the intestinal contents.
Serosa forms the mesentery on which the entire thin section is suspended. At the same time, the mesentery of the jejunum and ileum is better expressed, and therefore they are combined under the name mesenteric colon.
INTESTINAL FUNCTIONS
Digestion of food is completed in the small intestine under the action of enzymes produced by the wall ( liver and pancreas) and wall ( Lieberkühnand Brunner's) glands, absorption of digested products into the blood and lymph, and biological disinfection of incoming substances.
The latter occurs due to the presence of numerous lymphoid elements enclosed in the wall of the intestinal tube.
The endocrine function of the thin section is also great, which consists in the production of some biologically active substances by intestinal endocrinocytes (secretin, serotonin, motilin, gastrin, pancreozymin-cholecystokinin, etc.).
PARTS OF THE SMALL INTESTINE
It is customary to distinguish three sections of the thin section: initial segment or duodenum, middle segment or jejunum and the end segment or ileum.
DUODENUM
Structure
Duodenum- the initial section of the thin section, which is connected to the pancreas and the common bile duct and has the form of a loop facing caudally and located under the lumbar spine.
The duodenum accounts for 10% of the total length of the small intestine. This section of the thin section is characterized by the presence of duodenal (Bruner's) glands and a short mesentery, as a result of which the intestine does not form loops, but forms 4 pronounced convolutions.

Topography
The duodenum, leaving the stomach, rotates so that it forms an acute angle (cranial bend). Initially, it is directed caudally and slightly to the right, but soon acquires a caudal direction, located in the right hypochondrium. Approximately 10 cm caudal to the pylorus, the intestine makes a U-shaped bend, passing 4 - 5 cm forward and to the left, then passes into the jejunum without pronounced boundaries. Between the branches of the U-shaped bend is the duodenum of the pancreas. Approximately 3 cm from the pylorus, the intestine receives the common bile and pancreatic duct. At the confluence of the duct on the mucous membrane there is a small papilla, the apex of which bears an oval opening. The confluence of the accessory duct is located 2 cm caudal to the main pancreatic duct.
JEJUNUM
Structure
Jejunum- the longest part of the thin section. Makes up to 70% of the length of the thin section.
The intestine got its name due to the fact that it has a half-dormant appearance, that is, it does not contain voluminous contents. The diameter exceeds the ileum located behind it and is secreted big amount vessels passing through a well-developed mesentery.
Due to its considerable length, developed folds, numerous villi and crypts, the jejunum has the largest absorption surface, which is 4-5 times greater than the surface of the intestinal canal itself.
Endoscopy of the jejunum:

Topography
Its loops hang on the elongated mesentery and form numerous curls, occupying a vaguely defined area of the abdominal cavity. Caudally it passes into the ileum.
ILEUM
Structure
Ileum- the final part of the thin section, reaching a length of up to 20% of the length of the thin section. Its structure is no different from the jejunum. Its diameter is relatively constant, in the caudal part the walls are thinner. The ileum is characterized by the accumulation of numerous lymphoid elements that lie in its wall (Peyer's patches). In the right iliac region it flows into the colon, forming a valve (valve). The valve with its protruding part of the mucous membrane is directed into the lumen of the colon. In the area of the valve, the muscle layer is significantly thickened, the mucous membrane is free of villi. During normal peristalsis, the valve periodically expands and allows contents to pass into the large intestine.
Endoscopy of the ileum: 
Topography
The ileum is suspended on the folded mesentery. It is separated from the lower abdominal wall only by the omentum.
WALL GLANDS. LIVER
Liver- the largest gland in the body, it is a parenchymal organ of red-brown color. Its absolute weight in adult cats averages 95.5 g, i.e. 3.11% relative to the total weight of the animal.
Five tubular systems are formed in the liver: 1) bile ducts; 2) arteries; 3) branches of the portal vein (portal system); 4) hepatic veins (caval system); 5) lymphatic vessels.
Appearance of an isolated liver:

The shape of the liver is irregularly rounded with a thickened dorsal margin and sharp ventral and lateral margins. The pointed edges are dissected ventrally by deep grooves into lobes. The surface of the liver is smooth and shiny due to the peritoneum covering it, only the dorsal edge of the liver is not covered with peritoneum, which in this place passes onto the diaphragm, and thus is formed extraperitonealfield liver.
Located under the peritoneum fibrous membrane. It penetrates the organ and divides it into lobes.
The main sagittal notch divides the liver into right and left lobes; in the same notch there is a round ligament, the continuation of which is the falciform ligament connecting the liver with the diaphragm and the transverse coronary ligament.
Each lobe of the liver is further divided into medial and lateral parts. The left medial lobe is small. The left lateral lobe, which with its sharp end covers most of the ventral surface of the stomach, is significantly larger in size. The right medial (vesical) lobe is extensive, on its posterior surface there is gallbladder with the cystic duct. Right lateral lobe - located dorsal and caudal to the vesical lobe and is deeply split into caudal and cranial parts. The first is elongated and reaches the caudal end of the right kidney, adjacent to its ventral surface; the dorsal surface of the second is in contact with the adrenal gland. In addition to those listed, at the base of the right lateral lobe there is an elongated triangular caudate lobe; it lies at the omental sac and partially covers its entrance.
Schematic representation of the liver and gallbladder:

The liver is a polymer organ in which several structural and functional elements can be distinguished: hepatic lobule, sector, (a section of the liver supplied by a branch of the portal vein of the 2nd order), segment (a section of the liver supplied by a branch of the portal vein of the 3rd order), hepatic acini(adjacent areas of 2 adjacent lobules) and portal hepatic lobule(areas of 3 adjacent lobules).
The classic morphofunctional unit is hepatic lobule hexagonal in shape, located around the central vein of the hepatic lobule.
The hepatic artery and portal vein, having entered the liver, are repeatedly divided into lobar, segmental, etc. branches up to interlobulararteries and veins, which are located along the lateral surfaces of the lobules along with interlobularbile duct, forming hepatic triads. From these arteries and veins branches arise that give rise to sinusoidal capillaries, which flow into the central veins of the lobule.
The lobules consist of hepatocytes, which form trabeculae in the form of two cellular cords. One of the most important anatomical features of the liver is that, unlike other organs, the liver receives blood from two sources: arterial- along the hepatic artery, and venous- along the portal vein.
One of the most important functions of the liver is bile formation process, which led to the formation of the bile ducts. Between the hepatocytes forming the lobules there are bile ducts that flow into the interlobular ducts.
The interlobular bile ducts merge to form the hepatic excretory duct; there may be several of them. The excretory cystic duct also departs from the gallbladder; it connects with the hepatic duct, forming the common bile duct, which opens together with the pancreatic duct
into the duodenum. At the end of the bile duct lies the sphincter of Oddi, which also covers the pancreatic duct.
Gallbladder It is an elongated pear-shaped sac that lies in the cleft of the right medial lobe of the liver so that the apex is visible from the front. Its extended end is free and directed caudoventrally. When moving to its free end, the peritoneum forms 1 - 2 ligament-like folds. The length of the cystic duct is about 3 cm.
At the point where it enters the intestine, the duct has bile duct sphincter(sphincter of Oddi). Thanks to the presence of the sphincter, bile can flow directly into the intestines (if the sphincter is open) or into the gallbladder (if the sphincter is closed).
The anterior, or diaphragmatic, surface is slightly convex and adjacent to the diaphragm, the posterior, or visceral, surface is concave. The lateral and ventral edges are called the sharp edges of the liver, the dorsal edge is called the blunt edge of the liver. Most of the organ is located in the right hypochondrium. Approximately in the center of the visceral surface of the liver, vessels and nerves penetrate into it, and the bile duct emerges - this is the gate of the liver. The caudal vena cava passes along the blunt edge, fused with the liver. To the left of it is the notch for the esophagus.
Blood supply the liver receives through the hepatic arteries, portal vein, and venous outflow occurs through the hepatic veins
into the caudal vena cava.
Innervation The liver is supplied by the vagus nerve through the extra- and intramural ganglia and the sympathetic hepatic plexus, represented by postganglionic fibers from the semilunar ganglion. The phrenic nerve takes part in the innervation of the peritoneum covering the liver, its ligaments and the gallbladder.
LIVER FUNCTIONS
The liver is a multifunctional organ that takes part in almost all types of metabolism. The digestive function of the liver is reduced to the process of bile formation, which promotes the emulsification of fats and the dissolution of fatty acids and their salts. The liver plays a barrier and disinfecting role, is a depot of glycogen and blood (up to 20% of the blood is deposited in the liver), and in the embryonic period it performs a hematopoietic function.
In the animal body, the liver performs many functions, takes part in almost all types of metabolism, plays a barrier and disinfecting role, is a depot of glycogen and blood, and performs a hematopoietic function in the embryonic period. The digestive function of the liver is reduced to the process of bile formation, which promotes the emulsification of fats and the dissolution of fatty acids and their salts. In addition, bile increases the activity of enzymes in intestinal and pancreatic juices and stimulates peristalsis.
WALL GLANDS. PANCREAS
Pancreas flat, variable in outline, about 12 cm long, 1 - 2 cm wide, consists of individual small lobules connected into one whole by loose connective tissue, has a pale pink color.
Appearance of the pancreas:

According to the structure of the iron, it belongs to the complex tubular-alveolar glands of mixed secretion. The gland does not have clear contours, since it does not have a capsule, is stretched along the initial section of the duodenum and the lesser curvature of the stomach, covered with peritoneum ventro-caudally, the dorsal part is not covered with peritoneum.
The pancreas consists of exocrine lobules And endocrine parts.
Schematic representation of the pancreas:


Located in the initial loop of the duodenum. The gland is curved in the middle almost at a right angle: one half lies at the greater curvature of the stomach, its free end touches the spleen, the other half lies in the omentum of the duodenum.
There are usually 2 ducts in the gland. The main duct is short, formed as a result of the fusion of ducts that collect pancreatic juice from both halves of the gland; together with the common bile duct, it flows into the duodenum approximately 3 cm from its beginning. The accessory duct is formed as a result of the connection of branches anastomosing with the main duct; opens approximately 2 cm caudal to the main one, sometimes absent.
Blood supply The glands provide branches of the splenic, hepatic, left gastric and cranial mesenteric arteries, and venous drainage occurs in the portal vein of the liver.
Innervation carried out by branches of the vagus nerve and the sympathetic plexus of the pancreas (postganglionic fibers from the semilunar ganglion).
FUNCTIONS OF THE PANCREAS
The pancreas is responsible for both exocrine,
and for endocrine functions, but in the context of this section only exocrine digestive functions are considered.
The exocrine pancreas is responsible for secreting digestive hormones and large volumes of sodium bicarbonate ions, which neutralize the acidity of the chyme that comes from the stomach.
Secretion products:
Trypsin: breaks down whole and partially digested proteins
on peptides of various sizes, but does not cause the release of individual amino acids.
- chymotrypsin: breaks down whole and partially digested proteins into peptides of various sizes, but does not cause the release of individual amino acids.
- carboxypeptidases: breaks down individual amino acids
from the amino terminus of large peptides.
- aminopeptidase: breaks down individual amino acids
from the carboxyl end of large peptides.
- pancreatic lipase: hydrolyzes neutral fat
into monoglycerides and fatty acids.
- pancreatic amylase: hydrolyzes carbohydrates, converting them
into smaller di- and trisaccharides.
6. Large intestine (Intestinum crassum)
Schematic representation of the large intestine:

Colon is the terminal portion of the intestinal tube and consists of blind, colon And straight intestines and ends in the anus. It has a number of characteristic features, which include relative shortening, volume, and low mobility (short mesentery). The large intestine is distinguished by its width and the presence, on the border with the small intestine, of a peculiar outgrowth - the cecum. The cat has no muscle cords. The mucous membrane, due to the absence of villi, does not have a characteristic
for a slimy velvety feel.
Cross section of the colon wall

Large stenosing malignant tumor in the colon of an old cat with tenism and vomiting:

Blood supply The colon is supplied by the branches of the cranial and caudal mesenteric arteries, and the rectum is supplied with blood by three rectal arteries: cranial(branch of the caudal mesenteric artery), middle and caudal(branches of the internal iliac artery).
Venous drainage from the cecum, colon and cranial portion of the rectum occurs into the portal vein of the liver. From the middle and caudal portions of the rectus cat into the caudal vena cava, bypassing the liver.
Innervation the thick section is provided by branches vagus(transverse position of the colon) and pelvic nerves(blind, most of colon and rectum). The caudal part of the rectum is also innervated by the somatic nervous system through the pudendal and caudal rectal nerves of the sacral spinal plexus. Sympathetic innervation is carried out through the mesenteric and rectal plexuses, which are formed by postganglionic fibers of the semilunar and caudal mesenteric ganglia.
Muscle control from the nervous system is carried out both through local reflexes and through vagal reflexes involving the submucosal nerve plexus and the intermuscular nerve plexus, which is located between the circular and longitudinal muscle layers. Normal bowel function is regulated by the parasympathetic nervous system. Control is directed from the medullary part of the vagus nerve to the anterior part and from the nuclei of the sacral spine
through the pelvic nerve to the peripheral part of the large intestine.
The sympathetic nervous system (control directed from the ganglia in the paravertebral sympathetic trunk) plays a less important role. The processes of local control and coordination of motility and secretion of the intestine and associated glands are of a complex nature, involving nerves, paracrine and endocrine chemicals.
The loops of the large intestine are located in the abdominal and pelvic cavities.
Contrast radiography of the large intestine:

MININGS OF THE INTESTINAL
The structure of the large intestine consists of several layers: mucous membrane, submucosallayer, muscle layer(2 layers - outer longitudinal layer and inner circular layer) and serosa.
The epithelium of the cecum does not contain villi, but has numerous goblet cells on the surface that secrete mucus.
Mucous membrane It does not have villi or circular folds, which is why it is smooth.
The following types of cells are distinguished in the mucous membrane: intestinal epithelial cells with a striated border, goblet enterocytes, borderless enterocytes - the source of restoration of the mucous membrane, and single intestinal endocrinocytes. Paneth cells, present in the small intestine, are absent in the large intestine.
General intestinal(Lieberkühn's) glands are well developed, lie deep and close to each other and there are up to 1000 glands per 1 cm2.
The openings of the liberkühn glands give the mucous membrane an uneven appearance. In the initial part of the thick section, there is an accumulation of lymphoid elements that form plaques and lymphatic fields. An extensive field is located in the cecum at the confluence of the ileum, and plaques are located on the body of the cecum and at its blind end.
Muscularis in the thick section it is well developed, which gives the entire thick section a thick appearance.
FUNCTIONS OF THE LARGE INTESTINE
Undigested food debris enters the large intestine and is exposed to the microflora inhabiting the large intestine. The digestive capacity of the large intestine of cats is negligible.
Some excreta are released through the mucous membrane of the large intestine ( urea, uric acid) And salt heavy metals , mainly in the initial part of the colon, water is intensively absorbed. The thick section is functionally more of an organ of absorption and excretion than of digestion, which leaves an imprint on its structure
PARTS OF THE LARGE INTESTINE
The large intestine consists of three main parts: cecum, colon And rectum.
CECUM
StructureThe cecum is a blind outgrowth at the border of the thin and thick sections. The iliac foramen is well defined and represents an obturator mechanism.
The cecum has no locking mechanism
and is not clearly expressed. The average length of the intestine is 2-2.5 cm. Its structure resembles a short but wide pocket, ending with a pointed lymphoid end.
Topography
The cecum is suspended on the mesentery on the right in the lumbar region under the 2nd-4th lumbar vertebrae. The cecum forms a pouch, closed at one end, located below the junction of the large and small intestine. In cats, the cecum is a vestigial organ.
COLON
StructureColon - with a length (about 23 cm) and volume it represents main part large intestine. Its diameter is 3 times greater than the ileum, which flows into it at a distance of 2 cm
from the cranial end. The colon, unlike the small intestine, does not twist in loops. It distinguishes between the ascending, or right, knee, the transverse (diaphragmatic) knee and the descending, or left, knee, which goes into the pelvic cavity, forming a weak gyrus, after which it passes into the rectum.
Topography
The intestine is suspended on a long mesentery and runs in a simple rim from right to left.
RECTUM
StructureThe rectum is small (about 5 cm in length). The intestine has smooth, elastic and thick walls with a uniformly developed muscle layer. The mucous membrane is collected in longitudinal folds and contains modified Lieberkühn glands and numerous mucous glands that secrete large amounts of mucus. In the initial part it is suspended on a short mesentery; in the pelvic cavity it expands somewhat, forming an ampoule. Under the root of the tail, the rectum opens outward into the anus.
Topography
It lies under the sacral and partly under the first caudal vertebrae, ending with the anus.
Anus
The anus is surrounded by a double muscular sphincter. It is formed by striated muscles, the second is a continuation of the smooth muscle layer of the rectum. Besides,
A number of other muscles are attached to the rectum and anus:
1) rectocaudalis muscle represented by a longitudinal layer of rectal musculature, which passes from the walls of the rectum to the first caudal vertebrae;
2) lifteranus originates from the ischial spine and goes from the side of the rectum to the muscles of the anus;
3) suspensory ligament of the anus originates from the 2nd caudal vertebra and in the form of a loop covers the rectum from below.
Constructed of smooth muscle tissue. In males it passes into the retractor of the penis, and in females it ends in the labia.
The perineal part of the rectum is called anal canal. The mucous membrane ends near the anus with a ring anorectal line. The anus is delimited from the outer integument by a circular cutaneous-anal line. Between them in the form of a belt
with longitudinal folds there is a columnar zone.
On the sides of the anus in the sinuses, the anal glands open outward, secreting an odorous fluid.
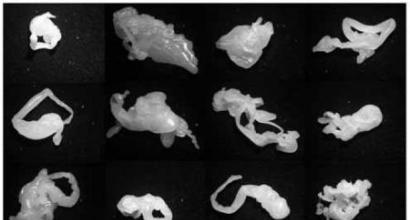
Objective data indicate high morbidity and high mortality in dogs and cats from gastrointestinal disorders. Adequate feeding, exercise, proper maintenance of mothers during pregnancy and good care for them have a great influence on the course of the growth and development of the fetus. Consequently, the prevention of gastrointestinal diseases in young animals should begin with creating conditions for normal intrauterine development and fetal growth.
Pathological changes in the stomach and intestines of dogs and cats develop quickly and involve almost the entire body in this process, therefore it is necessary to correctly diagnose and treat the animal at the earliest possible moment. early period diseases.
1. Gastritis, gastroenteritis and gastroenterocolitis.
The most common diseases of the gastrointestinal tract in dogs and cats include: gastritis (inflammation of the mucous membrane of the stomach), gastroenteritis (inflammation of the mucous membrane of the stomach and small intestine) and gastroenterocolitis (inflammation of the mucous membrane of the stomach, small and large intestine). In veterinary practice, the inflammatory process often covers the stomach and the entire intestine at the same time, spreading from top to bottom or bottom to top, and in this case is diffuse in nature.
The most common cause of acute inflammatory processes in the gastrointestinal tract is feeding with poor quality and unusual food for animals, such as spoiled fish, meat, sausage, sweets, canned food, butter, sour cream, cheese, stale lactic acid products, etc. Do not feed dogs and cats pork, lamb, drink cold, dirty or hot water. The microflora that populates the gastrointestinal tract increases its pathogenic properties in most cases when the body’s immune system is weakened, under the influence of unsanitary conditions.
Puppies and kittens often suffer from gastrointestinal problems during a rapid transition from mother's milk to self-feeding, during a sudden change in diet, in the absence of water, or when animals have to drink dirty water. Inflammation of the gastrointestinal tract occurs when eating feed with mechanical impurities (sand, earth, pieces of wood, glass, paper, etc.).
In dogs and cats, inflammation of the stomach and intestines occurs when poisonous plants, chemical and medicinal substances, and mineral fertilizers enter the food. Some dog and cat breeds are predisposed to food allergies.
In most cases, inflammation of the stomach and intestines occurs as a secondary process in a number of acute infectious, invasive and non-contagious diseases.
Among the infectious diseases of dogs in which inflammation of the gastrointestinal tract occurs, we should highlight, first of all, plague, parvovirus enteritis, infectious hepatitis, salmonellosis, colibacillosis, tularemia, leptospirosis, botulism, dysentery and mycoses, and in cats - panleukopenia and herpesvirus infection. Lesions of the gastrointestinal tract are often observed with piroplasmosis, cystoisosporosis, toxoplasmosis, helminthiases (nematodes, cestodiases).
Gastritis, gastroenteritis and gastroenterocolitis in dogs and cats arise as complications of some non-contagious diseases, such as poisoning, stomatitis, pharyngitis, periodontitis, mumps, peritonitis, inflammation of the esophagus, liver diseases, respiratory organs, sepsis, abdominal trauma and some surgical and obstetric - gynecological diseases.
In practice, acute gastritis and gastroenteritis often develop into a chronic form, which periodically worsens under certain unfavorable conditions and is accompanied by stomatitis.
Symptoms of gastritis. With acute gastritis in dogs and cats, lethargy, fatigue, sometimes a short-term slight increase in body temperature, signs of anxiety, especially after feeding, perversion of appetite (eating food unusual for the animal, licking walls, wallpaper, plaster, swallowing pieces of wood, stones, rags) are noted etc.), often its reduction, up to complete refusal of food.
Sick dogs and cats lose weight. The conjunctiva at the beginning of the disease is reddened (hyperemia), later becomes pale with a bluish tint, and jaundice often develops. The mucous membrane of the mouth is covered with viscous, viscous saliva, the tongue is gray or white coating. The smell from the mouth is sweetish, musty or putrid. Sometimes the onset of jaundice is more clearly visible on the sclera. The feces are compacted, dark in color, covered with a thin film of mucus.
A very characteristic sign of gastritis is the possible presence of belching, vomiting soon after eating and drinking, less often independently of them. Vomit is mixed with saliva and viscous gastric mucus, sometimes with blood, and with repeated vomiting - with bile. In the intervals between attacks of vomiting, some relief occurs, although the animal maintains a forced posture - arching its back, pulling its stomach, pressing its hind limbs to its chest. As a result of frequent vomiting, the body loses fluid. An external sign of dehydration is a decrease in skin turgor.
In chronic gastritis with high acidity, there is a weakening of intestinal motility and constipation. The amount of gastric contents on an empty stomach is increased, its general acidity is increased, more often as a result of increased formation of organic acids, in addition to the above symptoms, gas belching and vomiting may appear soon after eating food.
Symptoms of acute gastroenteritis and gastroenterocolitis usually increase rapidly. In dogs and cats, appetite disappears/thirst increases. Mobility and performance decrease sharply. The temperature rises to 40 "C and above. The general condition is characterized by depression, lethargy, signs of constant anxiety in the form of colic often appear. Animals groan or, conversely, are indifferent, lying more. Fibrillar muscle twitching is possible. The heart beat and heart sounds are increased. The pulse is increased. , arrhythmic. At the beginning of the disease, blood pressure rises briefly, then falls. Urination is rare.
In the subsequent development of the disease due to intoxication, depression increases, up to a coma. The hair becomes dull and the skin turgor is reduced. The stomach is tucked. Muscle tone weakens, the anal sphincter is relaxed. The body temperature is lowered, the limbs, ears, and nose become cold. Exhaustion develops.
Symptoms of chronic gastroenteritis and gastroenterocolitis. Chronic gastroenteritis and gastroenterocolitis are characterized by a very diverse and motley clinical picture, and it depends on the form of inflammation, the location and course of the pathological process. Important and constant signs of the disease are a gradual decrease in fatness, growth retardation compared to peers with relatively preserved appetite and sufficient feeding, general lethargy, normal temperature, decreased skin turgor, dull, uneven and tousled hair, delayed molting, pale visible mucous membranes, often bluish and icteric shades. The release of gases is constant, through belching. Vomiting often occurs. Feces, depending on the peristalsis of the small and large intestines, are dry or liquid, sometimes watery, with a putrid odor, containing a lot of mucus and undigested food particles.
With subsequent exacerbations, the clinical picture resembles the acute course of gastroenteritis and gastroenterocolitis.
Secondary acute and chronic gastroenteritis and gastroenterocolitis are complemented by clinical signs of the underlying disease.
Prevention. Prevention of gastrointestinal diseases can be general and specific. The basis of general prevention of young dogs and cats is biologically complete feeding, taking into account their physiological state, providing active exercise, maintaining good sanitary condition and microclimate in the places where the animals are located.
Poor quality and unusual foods (sweets, confectionery, foods high in fat, canned food, sausage, etc.) are excluded from the diet of carnivores. Feeding pork to dogs and cats is strictly prohibited. It is unacceptable to contain mechanical impurities, mineral fertilizers, herbicides, drugs and other toxic substances in feed. Animals should always have plenty of clean water at room temperature. It is advisable to feed animals 2-4 times a day without overloading the stomach. The change in diet should be gradual. It is necessary to periodically carry out preventive fortifications (after consultation with a veterinarian).
2. Gastric ulcer in dogs.
Peptic ulcer is a chronic relapsing disease in which, as a result of disruption of regulatory, nervous and hormonal mechanisms and gastric digestive disorders, a peptic ulcer is formed in the stomach and, less commonly, in the duodenum.
Long-term feeding of waste Catering mixed with large amounts of salt, mustard, pepper and other irritating substances, as well as numerous imported feeds and fertilizers - the direct cause of the formation of ulcers. Predisposes to the disease are disturbances in the feeding regime (long breaks in feeding, skipping regular feedings, etc.), feeding frozen fish, meat, hot food to hungry animals, exposure to stress (change of owner, violation of training methods, shouting, etc.). The disease in most cases occurs as a continuation of gastritis.
The course of the disease is chronic, with rare exceptions. Against the background of signs of chronic gastritis (deterioration or perversion of appetite, frequent regurgitation) in animals with the development of ulcers, the general condition worsens, weakness and depression appear, and emaciation quickly progresses. Characteristic sign- the appearance of vomiting several hours after eating food and the presence of bile and blood in the vomit.
With a long course of the disease, the patient’s condition may worsen, and then periods of exacerbation with a sharp deterioration appear again general condition and frequent vomiting of blood.
3. Intestinal obstruction.
Internal blockage of the intestines can occur as a result of stones, soil, rags, pieces of wood, bones and other objects. In cats common cause Intestinal blockages are a clump of fur and hair.
In the formation of intestinal stones, a combination of three factors is important: dysregulation of the digestive organs (secretion, motility, absorption, etc.), as well as long-term feeding with rough, homogeneous and low-nutrient feed. Metabolic diseases are also a prerequisite for the development of intestinal stones. In cats, a common reason for the formation of hairballs in the large intestine is metabolic disorders and a delay in the molting process.
Partial obstruction of the large intestines is manifested by periodic moderate anxiety. During pain-free periods, animals can take food and water; they often continue to pass gas and defecate. After 2-4 days, the animals lose their appetite, anxiety increases, the general temperature rises, and the pulse and breathing increase.
In dogs, when the small intestines are blocked, frequent vomiting occurs, appetite is disrupted, the animal is anxious or depressed; Intestinal flatulence develops, peristalsis weakens, and constipation occurs.
Many owners mistakenly believe that if a cat has nine lives, then they should worry when minor (at first glance) symptoms of the disease appear.
not really worth it. Cats, indeed, have great survivability in the most incredible situations. But that doesn't mean she can't die
never getting help from the person she loved.....
Be attentive to any symptoms of illness in your pet.
So, any owner should be able and know what needs to be done if...
If your cat has diarrhea or vomiting. Of course, this is not a reason to immediately run to the doctor. Unless you are absolutely sure that your cat has inhaled or ingested some kind of toxic substance. Poisoning by inhalation can be caused by carbon monoxide, the smell of paints and varnishes, the use of insecticides when treating the room, etc., etc.
Well, getting poison inside... it could be anything, from any household chemicals, which are found in abundance in every modern home, to taking seemingly ordinary food......
So, vomiting or diarrhea...
In case of one-time vomiting or short-term diarrhea (no more than two days), any owner can cope with the situation independently. But! Remember - diarrhea itself is not an independent disease; it is often a symptom of another, perhaps very dangerous disease. If diarrhea with mucus, with blood, very severe, with vomiting, is accompanied by a strong increase in temperature, if vomiting becomes uncontrollable - RUN to the doctor! Don’t be like those owners who spend hours sitting at the computer typing phrases like this into search engines: “The cat has not eaten for five days, is breathing heavily, does not move, vomiting, diarrhea, what should I do?”
Diarrhea
Diarrhea in cats is quite common. Contrary to popular belief, cats are happy to rummage through the trash can. And even adult cats can try and swallow small objects that may be inedible and even poisonous (you won’t believe it, but right now, while I’m writing, my little one pulled the remote control towards him remote control, grabbed the film from it with his teeth and dragged it into his mouth. Okay, I'm nearby, I took it. This is how we have them - they need constant supervision)))). Diarrhea can also be caused by a change in food. But the cause of a long-term disorder may be viral infections and liver diseases, inflammatory processes in the gastrointestinal tract, as well as tumors. Do not forget that with severe, prolonged diarrhea there is a large loss of water, this leads to dehydration of the body, and this, in turn, leads to a very rapid death of your pet.....
So, diarrhea...
What can you do? Place your cat on a daily fasting diet. When the first symptoms of the disease appear, you need to give the cat 1-3 tablets of activated carbon, be sure to give it plenty of fluids, you can brew some herbs: chamomile decoction, flax seed decoction. After a day, start feeding the cat rice water, boil the chicken, buy Vetom 1.1, add it to the food. Until your stool returns to normal, stick to the rice-chicken diet. It is also recommended to serve the homeopathic remedy Nux vomica-Homaccord. It is good to give your cat Smecta for diarrhea. Dilute 1/2 of the sachet with water. How much water is actually not so important - water is just a solvent, I dissolved it in 1/4 cup. And drink a teaspoon every three hours. It is impossible to be poisoned by Smecta, but be careful - do not give the drug if the diarrhea has stopped. A cat doesn't need constipation either.
If the diarrhea is severe, does not stop and lasts more than two to three days, and moreover, mucus or blood appears in it, immediately, without hesitation, see a doctor!!!
Failure to help a cat when SUCH symptoms appear leads to rapid dehydration and death of the pet.
Constipation
If a cat cannot go to the toilet “in a big way” for more than two days, it’s time to sound the alarm. Most often, constipation occurs when a large number of hairballs are ingested by the cat when washing itself, but it can also occur when the cat swallows small, indigestible objects.
What to do first: The best remedy is to give the cat regular Vaseline oil (one tablespoon). Vegetable oil cannot be used! It is also impossible to do an enema if you are constipated; it is unknown for what reason this trouble happened.
If constipation continues, you should take your cat to the veterinarian.
The main thing for constipation is to exclude intestinal obstruction.
Intestinal obstruction
Intestinal obstruction can develop in cats due to constipation (coprostasis), as a result of helminthic infestation, as well as due to swallowed objects (often a Christmas tree decoration in the form of “rain” or thread) or volvulus. Distinguish mechanical ileus, in which intestinal transit is blocked, and ileus functional or paralytic, caused by atony of the intestinal wall. Functional ileus can be observed in cases of peritonitis, dysotonomia (disturbance of the autonomic nervous system), or after general anesthesia.
Symptoms: the cat is depressed or, on the contrary, does not find a place for itself, it refuses food, an unpleasant odor emanates from its mouth, and vomiting appears. The stomach swells, the cat meows pitifully, rolls on the floor, trying to stretch its stomach, and looks back at its stomach.
What to do. Don't hesitate to take your cat to the doctor! In case of intestinal obstruction, urgent intervention by specialists is required. She needs to undergo an X-ray examination (differential diagnosis is supplemented by contrast radiography using barium).
Acute gastritis
Causes: poor quality food, change of feed, poisoning by certain medicines, overfeeding, not regular feeding, giving cold (from the refrigerator) or hot food, helminthic infestation.
Symptoms: The main symptom of acute gastritis is the appearance of sudden vomiting. The cat refuses food, hunches over when moving, groans, pain in the stomach area, and a grayish-white coating on the tongue is possible. There may be an increase in temperature, stool is often unformed, with mucus. Constipation is often replaced by diarrhea.
What to do: On the first day of illness, you can give cerucal (an antiemetic). Do not feed the cat for the first day, after which serve it mucous infusions (rice), boiled chicken meat, always for 3-5 days. In the future, if the food is digested, the diet can be gradually expanded, but in any case, you must adhere to a gentle diet for a month. It is advisable to switch to dietary food for a while (for example, use the medicinal line from Royal Canin or Hill’s). Most often, if you adhere to these recommendations, the manifestations of acute gastritis disappear already on the third to fifth day.
Chronic gastritis.
Chronic gastritis can be a consequence of acute gastritis. Also, the causes of chronic gastritis can be a stressful situation (exhibitions, change of housing, change of owner, nervous situation in the family where the cat lives), endocrine diseases (diabetes, hyperthyroidism), inflammatory processes (cholecystitis, pancreatitis, etc.) .
Symptoms: With chronic gastritis, the cat loses weight, bad breath appears, vomiting is usually single, diarrhea or constipation, belching, flatulence, pain in the epigastric region.
Treatment of chronic gastritis will be long-term and individual.
What to do: Diet - Meat and fish only boiled, mucous decoctions. Meals 5-6 times a day in small portions. Eliminate fiber and fatty foods. A good help to the general treatment regimen is the use of a homeopathic drug, Nux vomica-homaccord.
After a one-day fast for your pet, it is necessary to serve decoctions of herbs such as chamomile, yarrow, St. John's wort, and flax seed.
It is advisable to show the cat to a veterinarian.
Gastroenteritis.
Gastroenteritis is inflammation of the stomach and small intestine. Has much in common with acute gastritis. Occurs as a result of excessively greedy food intake and stomach fullness, and can also be observed with some infectious diseases, such as panleukopenia, salmonellosis.
Symptoms: It is quite acute. There is a complete refusal of food, vomiting, diarrhea, rapid weight loss, the mucous membranes of the oral cavity are red, the nose is dry and warm, fever and severe thirst may be observed.
Feces with catarrhal inflammation are liquid, watery, fetid, mixed with undigested food and mucus.
What to do: Diet. During the first 24 hours, do not feed the cat, give only water, or better yet, herbal decoctions and infusions. It is advisable to give an injection of Gamavit, buy Vetom-1.1 at the pharmacy, add it to your cat’s food. For the first 3-5 days after a daily fast, serve mucous decoctions; it is recommended to give raw, fat-poor meat.
Necessarily Show the cat to the veterinarian.
The cause of intestinal dysfunction in cats can be feeding errors (mainly overeating, excess carbohydrates, fats), primary increased peristalsis (especially in very active animals). This phenomenon is not pathological and does not require treatment. You need rest and a diet in the form of one fasting day, deprivation of fluid for several hours, which is especially important when vomiting at the same time, then gradually begin to give the phytoelite cleansing tea as directed. If the animal does not drink on its own, the drug is given in the form of tablets; if water consumption is not impaired, it is better to give the drug dissolved in water. Feeding begins in small doses. Well-cooked, finely chopped meat with rice is best.
Inflammatory bowel disease in cats is mainly associated with chronic diarrhea (infections), malabsorption (malabsorption), anemia and weight loss (autoimmune diseases). It is difficult to treat.
Symptoms and treatment. In case of damage to the small intestine, characterized by infrequent stool with a large amount of fecal matter, the phytoelite “Protection against infections”, “Cleansing tea”, the use of only immunoprobiotic drugs - lactoferon, bactoneotime according to the treatment regimen, neoferon injection according to the treatment regimen, Vetom-1.1 are indicated.
Diarrhea due to infections of the large intestine (frequent stool with a small amount of feces) requires cleansing tea, bifid-containing probiotics - lactobifide, neotime or neoferon injection according to the treatment regimen.
In all cases, conventional therapy is indicated, aimed at restoring the water-salt balance, symptomatic remedies, and a gentle diet. The use of oral antibiotics is not recommended; they are often ineffective and cause dysbiosis.
Chronic diseases of the small intestine are digestive disorders and malabsorption (malabsorption). The cause of the disease may be a deficiency of pancreatic enzymes, bile and excessive development and disruption of the species composition of the intestinal microflora. Symptoms The disease is expressed in exhaustion, dehydration, ascites, and decreased appetite. The coat is dull. The prognosis is cautious; the disease is practically incurable.
Treatment. Symptomatic and supportive treatment can be provided.
With malabsorption in cats, a phenomenon called "greasy tail" is often observed. A positive effect of a course of antibiotics on the outcome of the disease was noted. However, with this treatment the disease is recurrent. It is more effective to use drugs containing pancreatic enzymes - panzinorm, etc. There is evidence of positive impact on the course of the disease when feeding animals with yogurt prepared with lactobifide.
The main direction of treatment for malabsorption is fractional dietary nutrition in small portions - complete protein, lean meat, for example, boiled chicken, cottage cheese, adding raw bran, Hill's Pet Products food. Vitamin supplements are not recommended for healthy animals, as they can stimulate the development of microflora. You can use restorative phytomins. The use of probiotics without an immunomodulator in this case gives practically no results and can even worsen the animal’s condition. The disease cannot be completely cured, however, it can be kept under control.